Contact lens forums are filled with comments from hard contact lens wearers complaining about lens fogging. Many are simply annoyed, but some reach the point where they cannot see through the fog. Most have no idea what causes it or what to do about it.
Discussing Scleral Lens Fogging with Dr. Tom Arnold
 We consulted with Dr. Tom Arnold of Today’s Vision Sugar Land, in Sugar Land, Texas, a leading optometrist specializing in custom contact lenses, to ask him more about lens fogging with rigid lenses and how he handles it with patients. Lens fogging is a function of deposits from the tear film sticking to the contact lens. Tear film traditionally has been thought of as three distinct layers of liquid but today the modern view is that there are approximately fifteen sublayers. On top, there is a lipid layer produced by the Meibomian glands located in the eyelids. Next, there is the aqueous or water layer which is what we commonly think of as tears. Lastly, the mucous layer produced by the goblet cells, actually coats the surface of the cornea, making it wetter and less hydrophobic.
We consulted with Dr. Tom Arnold of Today’s Vision Sugar Land, in Sugar Land, Texas, a leading optometrist specializing in custom contact lenses, to ask him more about lens fogging with rigid lenses and how he handles it with patients. Lens fogging is a function of deposits from the tear film sticking to the contact lens. Tear film traditionally has been thought of as three distinct layers of liquid but today the modern view is that there are approximately fifteen sublayers. On top, there is a lipid layer produced by the Meibomian glands located in the eyelids. Next, there is the aqueous or water layer which is what we commonly think of as tears. Lastly, the mucous layer produced by the goblet cells, actually coats the surface of the cornea, making it wetter and less hydrophobic.

Within those three layers, you have the sublayers that contain a variety of materials that can stick to lenses. Tears have proteins, immunoglobulins, oils, lipids, glycoproteins – all sorts of substances that can adhere to the surface of a contact lens. We blink about 12,000 times a day, and every time we do, we add a fresh layer of these products to the eye.

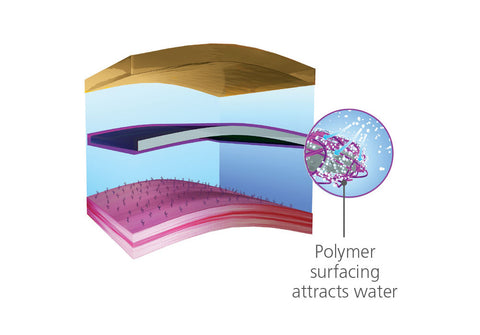
Rigid contact lenses are inherently hydrophobic, meaning they repel water, making them susceptible to collecting this material on their surface. At the same time, and surprisingly to many people, the surface of the cornea is not smooth; it is actually quite rough on a microscopic level.
What this looks like to patients is similar to a smudge on your eyeglasses, except that you can easily clean your glasses. With contact lenses, you may be looking through an oil slick and have a coating of mucous or protein on your lenses by the end of the day. Having to stop, remove the contact lenses, and proceed to clean them is simply not an option in most environments.
The patients that have the biggest problem with fogging, or deposits, tend to be scleral lens wearers. Patients that require this type of lens have a variety of conditions. This may include such things as ocular surface disease, keratoconus, post-refractive ectasias, trauma or simply a high ametropia. The deposits that they produce are significant and build up over time. That time frame may be a day, a week or a month. At the very least, these deposits may shorten the life of the lenses. On behalf of our patients we need to find a way to minimize, or even prevent, these deposits. We may fight it with hygiene. We ask our patients to scrub their lids, and perhaps give them a heat mask to use at night. We may prescribe supplements, like omega-3 fish oil, to improve the quality of their tear film. We struggle with it as do our patients because it can be a complicated regimen. And the simple fact is that many patients fail to be compliant with this care over the long term because of the complexity.
So, for me, ultimately it all comes down to this – how can we provide clarity and comfort of vision to our patients?
The Improvements Tangible Hydra-PEG Makes to Scleral Lenses
Rigid contact lenses are inherently hydrophobic, meaning they repel water, making them susceptible to collecting this material on their surface. At the same time, and surprisingly to many people, the surface of the cornea is not smooth; it is actually quite rough on a microscopic level.
 Scleral lenses can cost several hundred dollars or more apiece and often only last a year due to deposit build-up. Because of the expense, patients want their lenses to last as long as possible. Some people have very clean tears, and other people have very turbid or murky tears, so it is difficult to say from patient to patient how long lenses will last. However, in my practice, I have seen people with very challenging conditions using the Tangible Hydra-PEG coated lenses. When they follow our care regimen and recommendations, the benefits are extending the life of the lens. They look good, they stay clean and that is almost unheard of for many of these patients.
Scleral lenses can cost several hundred dollars or more apiece and often only last a year due to deposit build-up. Because of the expense, patients want their lenses to last as long as possible. Some people have very clean tears, and other people have very turbid or murky tears, so it is difficult to say from patient to patient how long lenses will last. However, in my practice, I have seen people with very challenging conditions using the Tangible Hydra-PEG coated lenses. When they follow our care regimen and recommendations, the benefits are extending the life of the lens. They look good, they stay clean and that is almost unheard of for many of these patients.
With traditional rigid lenses you have a daily cleaner, a disinfecting solution and possibly an enzymatic protein remover. All of those products are expensive, so there is a substantial cost burden to the patient to maintain their uncoated lenses.
Because lenses with Tangible Hydra-PEG are so effective in preventing deposits, patients have a much easier and less expensive care regimen. Generally, it involves just a conditioning/ disinfecting solution and sterile saline. That care burden is lifted from the patient and will likely improve compliance. What daily disposables did for soft contact lenses, Tangible Hydra-PEG is doing for the rigid lens universe. There is no substitute for a clean, wettable lens. I am confident in prescribing Tangible Hydra-PEG for my scleral patients, as well as for other lens types. The result is better vision and lenses that may last longer. They are usually more comfortable, especially for the dry eye patient. Money is saved on solutions. And the care burden is half that of uncoated lenses.
Dr. Arnold is a tireless advocate for his patients, and we appreciate his time and involvement in this post.
About Dr. Arnold
Dr. Thomas P. Arnold is a 1984 graduate of the University of Houston College of Optometry and owner of Today’s Vision Sugar Land since 1992. He holds a Bachelor of Science from the University of Northern Colorado and finished his pre-medical requirements at the University of Colorado at Boulder. Dr. Arnold completed his externship at the Indian Health Hospital in Santa Fe, New Mexico and was a research associate at The University of Texas Medical School for the Early Treatment of Diabetic Retinopathy (ETDRS) for the National Eye Institute. He has been a member of the Board of Directors of the Laser Eye Institute of Houston and adjunct facility at the University of Houston College of Optometry.




0 comments